Estimated reading time: 7 minutes
Key takeaways
- Women experience hormonal fluctuations throughout their lifespan, which can impact mood and sleep.
- GABA for women plays a crucial role as it may offer non-habit forming solutions for mental well-being.
- The gut microbiome significantly influences hormone levels, which in turn affects GABA levels and overall mental health.
- Supplements like GABA may help alleviate mood swings and improve sleep, particularly during hormonal transitions.
- Probiotic strains, such as Lactiplantibacillus plantarum, LP815, may enhance GABA production and support women’s mental health.
The Power of Microbes
Over the course of their lives, women go through several phases of hormonal fluctuations related to puberty, menstruation, pregnancy, and menopause. Since hormones are chemical messengers that help the body perform many functions, it’s natural that hormonal fluctuations could affect things like mood and sleep. In the U.S. more than half of women experience stress, sleeplessness, and unwanted mental health symptoms. GABA for women is an important consideration, as it may offer non-habit forming interventions to improve overall well-being.
One way scientists are doing this naturally is to look at the gut microbiome, or the microbes that normally reside in the digestive tract. These microbes perform many functions and have been shown to affect digestion, immunity, and even hormone levels. In this article, we take a look at the changes that occur in a woman’s lifespan and how we can support the relationship between hormones, neurotransmitters, and the gut microbiome.
Fluctuating Hormones Across Life Stages
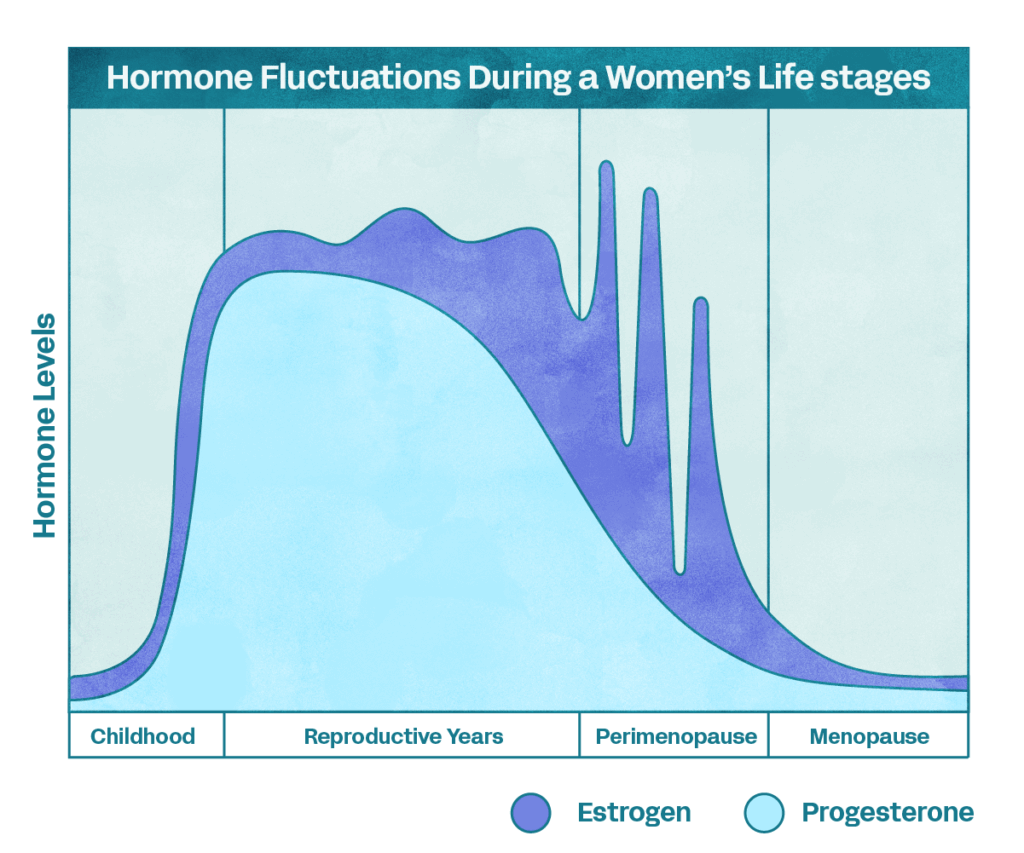
The sex hormones, estrogen and progesterone, fluctuate monthly during menstruation with even larger changes happening in pregnancy and menopause. The routine variations over menstruation can lead to premenstrual symptoms (PMS) and premenstrual dysphoric disorder, which is more severe than PMS. In pregnancy, hormone levels rise dramatically. Estradiol, a type of estrogen, increases to 50 times compared to its peak during the menstrual cycle and progesterone rises to 10 times higher than its peak during the menstrual cycle. During perimenopause and menopause, these hormones plummet leading to forgetfulness, mood changes, anxiety, and feelings of low energy.
How Do Hormonal Fluctuations Affect GABA?
The changes in mood happen because these hormones affect the levels of neurotransmitters such as gamma-aminobutyric acid (GABA), and the “happy hormones” serotonin and dopamine. GABA is an inhibitory neurotransmitter that calms the mind by preventing neuronal excitability. Acting at the other end of the spectrum is glutamate, an excitatory molecule. The ratio of glutamate to GABA, known as the E/I balance, is important as altering the balance can lead to anxiety and psychiatric disorders.1
We see GABA fluctuate during the menstrual cycle, with peaks in the prefrontal cortex of the brain during ovulation and dips during the luteal (premenstrual) phase.2 GABA levels decrease during perimenopause through menopause. More dramatic decreases during perimenopause are linked to depression and decreases in GABA in the hippocampus, a brain region associated with learning and memory, correlates with decreased memory in post-menopausal women.3,4
How the Body Responds to GABA:
While the amount of GABA itself matters, how well the body responds to GABA is also important. Both estrogen and progesterone are significant here because of their effects on brain cell receptors that help the cell respond to GABA. For example, progesterone breaks down into metabolites that affect how well receptors respond to GABA. Some of these metabolites positively modulate the receptor but other progesterone metabolites negatively affect it. Estrogen also decreases GABA activity by shortening how long GABA receptors are rooted in the communication points between brain cells.5
Because of the correlations between hormonal levels and GABA fluctuations, is it possible that supplementing with GABA can help with mood swings associated with hormone levels? It’s currently unclear how much ingested GABA actually makes it into the brain, but several studies have found benefits in taking GABA supplements. Taking GABA improves sleep by helping people fall asleep more quickly.6 The calming effects of taking GABA orally can be seen just one hour after ingestion and GABA seems to help with immunity under stress.7
What Does the Gut Microbiome Have To Do With It?
When it comes to the gut microbiome, we often think about its effects on our digestive health. But the gut microbiome influences much more than that. Via bi-directional communication with the brain, skin, and other organs, the gut microbiome seems to have a “say” in everything that goes on in our bodies.
Research finds that gut microbes have an important role in regulating estrogen and progesterone levels, which can then affect GABA levels and mental wellness. Evidence of this can be found in certain bacteria that produce enzymes that promote estrogen reabsorption into the bloodstream.8 Other studies find a bidirectional effect: changes in the gut microbiome have effects on estrogen levels and vice versa.9 Microbiomes look different in women who take hormonal contraceptives versus those who do not and women who have low, medium, or high levels of estradiol have differences in their gut microbes.10,11
Targeting the Microbiome: GABA for Women
Microbiome-targeting interventions are an evolving area of research, and there’s a growing body of evidence showing how the microbiome can support mental wellness. For example, certain gut microbes seem to improve mood and reduce anxiety while other strains produce GABA in the body.12,13
One such strain is Lactiplantibacillus plantarum, the bacterium at the core of Verb’s GABA LP815 probiotic. By producing GABA directly in the gut, probiotic bacteria can help relieve tension, stress, and sleep trouble during PMS and menopause. We’re excited to see the potential that GABA probiotics have on women’s health and how taking care of our gut microbes can lend itself to better mental wellbeing during periods of hormonal transitions.
About the Author
Jennifer Tsang, PhD is a microbiologist turned freelance science writer whose goal is to spark an interest in the life sciences. She works with life science companies, nonprofits, and academic institutions on anything from news stories, explainer articles, and content marketing. She shares the wonderful world of microbes on her blog The Microbial Menagerie. Learn more about Jennifer on her website jennifertsangwrites.com.
Sources:
- Hewett, S.J. et al. Influence of glutamate and GABA transport on brain excitatory/inhibitory balance. Exp Biol Med 246(9):1069–1083 (2021).
- De Bondt, T. et al. Prefrontal GABA concentration changes in women—Influence of menstrual cycle phase, hormonal contraceptive use, and correlation with premenstrual symptoms. Brain Res 1597:129-38 (2015).
- Tran, K.H. et al. Decreased GABA+ Levels in the Medial Prefrontal Cortex of Perimenopausal Women: A 3T 1H-MRS Study. Int J Neuropsychopharmacol 26(1):32–41 (2022).
- Jiménez-Balado, J. et al. Reduced Hippocampal GABA+ Is Associated With Poorer Episodic Memory in Healthy Older Women: A Pilot Study. Front Behav Neurosci 15:695416 (2021).
- Mukherjee, J. et al. Estradiol modulates the efficacy of synaptic inhibition by decreasing the dwell time of GABAA receptors at inhibitory synapses. Proc Natl Acad Sci U S A 114(44):11763-11768 (2017).
- Yamatsu, A. et al. The Improvement of Sleep by Oral Intake of GABA and Apocynum venetum Leaf Extract. J Nutr Sci Vitaminol (Tokyo) 61(2):182-7 (2015).
- Abdou, A.M. et al. Relaxation and immunity enhancement effects of gamma-aminobutyric acid (GABA) administration in humans. Biofactors 26(3):201-8 (2006).
- Kwa, M. et al. The Intestinal Microbiome and Estrogen Receptor–Positive Female Breast Cancer. J Natl Cancer Inst 108(8):djw029 (2016).
- Maeng, L.Y. et al. Never fear, the gut bacteria are here: Estrogen and gut microbiome-brain axis interactions in fear extinction. Int J Psychophysiol 189:66-75 (2023).
- Sinha, T. et al. Analysis of 1135 gut metagenomes identifies sex-specific resistome profiles. Gut Microbes 10(3):358-366 (2019).
- Shin, J.H. et al. Serum level of sex steroid hormone is associated with diversity and profiles of human gut microbiome. Res Microbiol 170(4-5):192-201 (2019).
- Rao, A.V. et al. A randomized, double-blind, placebo-controlled pilot study of a probiotic in emotional symptoms of chronic fatigue syndrome. Gut Pathog 1(1):6 (2009).
- Barrett, E. et al. γ‐Aminobutyric acid production by culturable bacteria from the human intestine. J Appl Microbiol 113(2):411-7 (2012).
Last Modified: